Frank O’Hagan
Introduction
This article has been written in a personal capacity and also incorporates perceptions gathered from other caregivers. Much could be mentioned concerning the multi-faceted contributions of Allied Health Professionals (AHPs) when assisting persons experiencing various forms of frailty and neuro-degenerative conditions, such as dementia and Parkinson’s Disease, and their carers. However, to examine them all is well beyond the aims and scope of a brief paper. Furthermore, research relating to improving health performance can be very complex but worthwhile (Chalmers and others, 2023). Rather, after commenting on AHPs’ overall involvement in various aspects of promoting healthier and happier standards of living, the main theme is a discussion on how some key areas of their work might usefully be taken forward.

A philosophical perspective on enriching lifestyles
Contemporary society requires to endorse an authoritative voice on behalf of services which prolong ‘quality-adjusted life years’ (QALYs). This movement underlines the advantages of both extending worthwhile everyday procedures and boosting good brain health. Rather than being wedged within a narrow medical model, there have been transformational changes towards what can be viewed as more personalised bio-psycho-social approaches. These concentrate directly on addressing the identified needs of both individuals and groups. There is an acceptance that all and sundry are different and that differing traits are acknowledged. Approval across diversity is recognised, validated, and celebrated. In advocating this climate for advancement, AHPs have been involved in developing beneficial initiatives and community-based programs to foster both physical and mental health.
There are many forms of interventions and support which can pause, reduce, or even reverse, rates of cognitive deterioration. Although, in the main, neuro-degenerative diseases are deemed as presenting intellectual and social challenges for older age groups, population statistics point to a wider ageing spectrum than is commonly supposed. Decision-making should be based on the ‘double empathy’ principle – in this case, a collaborative ‘coming together’ of the needs and wishes of persons experiencing disabilities and family caregivers in conjunction with the judgements and competences of professionals. Relationships should successfully combine the lived experiences, self-advocacy, and proposals of the former alongside curative and therapeutic procedures prescribed by the latter.
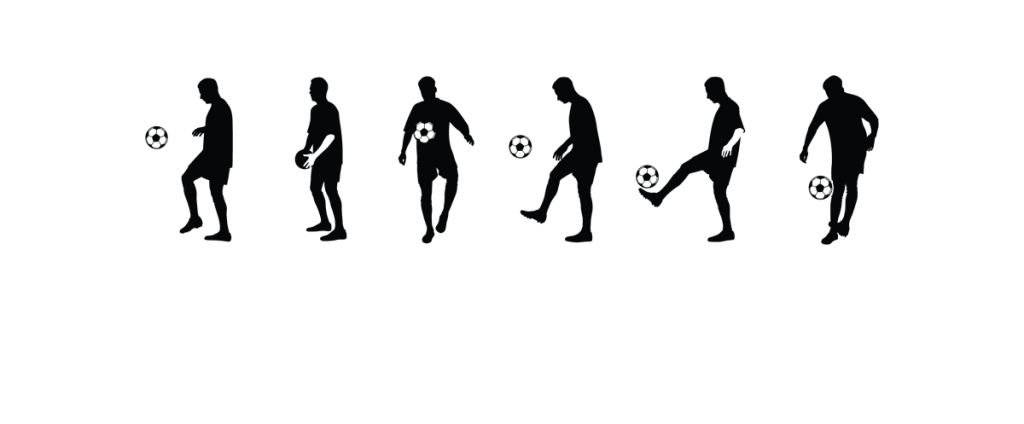
As implied earlier, a central characteristic of AHPs’ work is all about the pursuit and enrichment of the common good. This calls for comprehension and aptitude which are essential in effectively undertaking specific tasks. It also requires a range of suitable personal attributes such as thoughtfulness, compassion, open-mindedness, tolerance, and integrity. A focus on inclusiveness means that no one will be marginalised or disregarded. In addressing the needs, interests and benefits of individuals, a genuine sense of awareness, responsiveness, and care will have much to offer in strengthening dexterity and confidence. Innovations and training in features across dieting, fitness, movement, communication, technology, art, and music have brought to light the hidden, imaginative, and creative potentials of participants who previously had been ignored or ostracised. There is certainty that participatory physical, technological, and arts-based options can offer restorative experiences and augment emotional feelings.
“It is time to recognise the powerful contribution the arts can make to health and wellbeing.” (All Party Parliamentary Group on Arts, Health and Wellbeing, 2017)
Pathways towards further advancements
Although in recent years there has been a great deal to commend, there remain issues to grapple with and topics to examine in order to ensure that adeptness and productivity are enhanced. During the examination of five interrelating areas, it is proposed that the following pertinent questions are kept in mind. (a) While the responsibilities of AHPs are rightly regarded as focussing on health and wellbeing, would it be even more appropriate to emphasise and include ‘healing’ and ‘therapy’ as essential components? (b) Would the motif of ‘Promoting healing, therapy, health, and wellbeing’ seem applicable and all-encompassing? (c) Is the expertise of AHPs potentially untapped and their services underrated? (d) How can sensitive, flexible, and considerate interventions be developed to enhance future provision for those in need of assistance?
1: Establishing more collaborative networking
There are three aspects of fostering multidisciplinary alliances which are worthy of deliberation, namely – with carers and their families; between AHP groups within the same service; and connections across service providers.
From the standpoint of caregivers there can be both gratitude for the contributions of AHPs but simultaneously a realisation that their involvement is not well understood. In particular, there could be a lack of clarity vis-a-vis their functions and responsibilities. Often many carers do not know about them and others discover their relevance by accident. A great many people who require support belong to what is often referred to as the Silent Generation (persons born between 1927 and 1947). They, and other generations, can be ill-informed on the services obtainable or be hesitant to ask. There would be advantages in publicising policies and the availability of support more widely, including before a diagnosis of any distressful ailment is confirmed, to broaden caregivers’ capabilities and insights.
There also appears to be an interest on how there might be improvements in collaborative practices both between various AHP groups within a service and also across the boundaries of their employers. Pressures resulting from future budgeting may well affect the recruitment, coaching, and availability of frontline personnel. The consequences may necessitate the need for additional joint training and innovation. Evaluation leading to improvement will entail examining and auditing various factors such as how time is spent, the effectiveness of planning, the usage of resources, the number of carers and families involved, and feedback from all staff and participants. The overall aim of these tasks would be to take forward the proficiency of professional roles and making known their worth in maintaining wellbeing (Alzheimer Scotland, 2020).
2: Utilising expert knowledge and applying specialist skills
There will always be a requirement to constantly review abilities and to learn about up-to-date research findings on both the acquisition and application of evidence-based routines. Inevitably, there will be a wide continuum of criteria and quality regarding courses being offered within and between providers. Study and professional guidance are essential for the reinforcement of high professional standards (Healthcare Improvement Scotland, 2023).As indicated earlier, there is substantial scope for more collaborative continuing professional development focussed on assessment, counselling, and therapeutic interventions among AHPs. Perhaps the adoption of a COM-B model – with an emphasis on capability, opportunity, and motivation – will facilitate the identification of barriers and increase impactful professional practices. A worthwhile venture is to ascertain what have been termed ‘islands of excellence’ – examples of outstanding projects, methods and schemes which are verified as highly successful in sustaining healthier, societal self-assurance. There is considerable scope for practitioners to learn from such exemplars. Generously shared, observation of and training in ‘what works’ have much to offer.
3: Delivering inclusive and empathetic approaches to carers and disadvantaged persons
In line with what has been stated, many of those in need of relief, especially when confused and under pressure, are often unaware of what backing or funding might be available to them or even to whom they can turn to for advice and guidance. They require to be informed apropos the skillsets and availability of AHPs. Thoughtfulness and good sense will circumvent explanations which are too complicated for the listener or terminology which cannot be understood.
It also is the case that carers often complain about having to repeat their worries over and over again to professionals. As facilitators, AHPs can complement other groups’ participation within what can appear to outsiders to be a very convoluted social care system. Careful listening and clarification of any misapprehensions enhance collaboration and help avoid potential accidents or disagreements. The importance of the impact of public interactions and connectedness on psychological functioning and good mental health is beyond doubt. The old Latin adage “Nihil de nobis, sine nobis” (“Nothing about us, without us”) is frequently used in modern times by marginalised groups.Itremains highly apposite in the everyday affiliations which AHPs establish and maintain. When they are involved in direct support and proactive interventions, good practice necessitates that they confer closely with vulnerable people and carers, seek their views concerning previous oversights, help them to combat humiliation, and involve them in administrative matters.
“People with dementia and carers are keen to see the development of new approaches to person-centred care based on human rights principles of dignity and respect.” (Alzheimer Scotland, 2024)
There is clearly a role for AHPs to act as consultants in lessening apprehensions and anxieties while building self-esteem, fortitude, and resilience among carers. Due partly to the paucity of staff in some localities, proficiency in demonstrating procedures and ‘giving away skills’ is necessary in order for carers to undertake their own responsibilities more independently and effectively. In doing so, well-judged consideration of differing requirements will need to be taken as ‘one size fits all’ stratagems are generally unsuitable and misplaced. Working better together will result in greater efficiency, bolster community-based provision, and earn the admiration and trust of those who require assistance.
4: Providing high-quality, person-centred assessment
Currently, more discerning benchmarks are required at a national level pertaining to the evaluation of needs and subsequent planning for those experiencing cognitive ailments. Patience is critical in ensuring that recommended programs are firmly based on research and professional experiences. When collecting relevant personal information and identifying distinctive requirements, what might appear to be ‘a kaleidoscope of needs’ is revealed. Well-chosen targets and markers for progress hopefully will emerge and be articulated in a nuanced manner. Depending on circumstances, different types of assessments may be utilised. For example, self-referenced assessment to evaluate abilities against their previous levels across a designated period of time, or goal-based assessment to record the reaching of targets which previously had been set and understood by individuals or groups. Irrespective of the forms of valuation which are used, the spotlight must remain on living well, securely, and contentedly.
It is generally conceded that the frail and troubled exhibiting reduced brain health frequently have been neglected or overlooked with regard to a timely diagnosis. The sooner appropriate action is taken, the better. A well-tailored, personalised plan should be created and activated after the needs of individuals have been carefully and fully reviewed. Even when implemented, it is only to be expected that, at times, reactions to scheduled support and interventions may differ from intended outcomes or predictions. The suggestions from persons being helped and their carers are crucial when short- and long-term aims and goals of plans are being devised. These should cover recognised strengths and positive proposals for future development. Features of this process entails competent decision-making and the appraisal of contexts such as financial difficulties, inadequate living accommodation, environmental hazards, and mental health when deliberating on factors relating to risk and prevention. (Healthcare Improvement Scotland, 2023 and 2024; Livingston and others, 2024).
“We know that social isolation and loneliness is bad for our health, both mental and physical. It is essential that we recognise who in society is most affected and focus our efforts to tackle these inequalities.” (Scottish Government, 2023)
5: Highlighting progress and attending to regression
The monitoring of national strategies and policies from across Europe clearly indicates that there are ongoing inequalities connected with dementia care and treatment. (European Dementia Monitor Report, 2023). There also should be recognition that there are significant disparities within individual nations regarding backing for all forms of deteriorating mental health.
The insightfulness and collaboration of AHPs and family carers can be highly productive in detecting the complex nature of an individual’s obstacles and setbacks. Together, they can pinpoint unintended consequences of potentially harmful habits and formulate helpful solutions to mitigating and overcoming potential dangers in both home and local environments. Clearly, stimulating teamwork can enrich the daily routines of persons experiencing dementia through finding profitable ways to thwart relapses.
First-rate monitoring will provide substantial information, feedback, and guidance to augment the effectiveness of mediation and aid. Frequently, there is a need to update scheduling based on the progress or regression which has been measured or observed. The rationale may be that advances, even when confirmed, are slight or exceedingly non-linear. Alternatively, on occasions, more challenging modifications to what had previously seemed suitable may now be necessary because of rapid, flourishing headway and unexpected accomplishments. When detected, all achievements should be acknowledged, recorded, and commended.
Summary and concluding comments
The competences, know-how, and programs of AHPs are of great value and much appreciated by family carers. Active listening and mutual exchanges can be the foundation on which feelings of empathy, confidence and security are reinforced. Their long list of welcomed undertakings can include endeavours in enhancing: self-assurance; trust; interpersonal relationships; communication; household safety measures; physical vigour; mental health; and empowerment. Additionally, the characteristics of successful participation may embrace: taking full account of subjective experiences; demonstrating tactics to relieving stress; carrying out salutary tasks concerning the anticipatory/pre-death grief of carers; alleviating troubles and angst following the bereavements of loved ones; providing advice on connectedness with nature and the benefits of making good use of green spaces; and the employment of humour and novelty when appropriate.
The role of AHPs in promoting positive and fulfilling lifestyles for loved ones is cherished and respected by caregivers. As recipients continue to receive valued assistance and realise the benefits of individualised, group and communal inputs, they will wish to have more access to the services of AHPs. It is suggested that further developments along the lines outlined in five inter-connected areas, namely:(1) establishing more collaborative networking; (2) utilising expert knowledge and applying specialist skills; (3) delivering inclusive and empathetic approaches to disadvantaged persons and carers; (4) providing high-quality, person-centred assessment; (5) highlighting progress and attending to regression; will further advance the quality, efficiency, and outcomes of their contributions.
References
1. All-Party Parliamentary Group on Arts, Health and Wellbeing (2017) Inquiry Report Creative Health: The Arts for Health and Wellbeing. Second Edition.
2. Alzheimer Scotland (2020) Connecting People, Connecting Support – Transforming the allied health professionals’ contribution to supporting people living with dementia in Scotland, 2017-2020.
3. Chalmers S, and others (2023) The value of allied health professional research engagement on healthcare performance: a systematic review. BioMed Central Health Services Research, 23, Article number 766.
4. Scottish Government (2023) Social isolation and loneliness: Recovering our Connections 2023 to 2026.
5. Healthcare Improvement Scotland (2023) Scottish Intercollegiate Network SIGN 168 Assessment, diagnosis, care and support for people with dementia and their carers.
6. European Dementia Monitor Report (2023) – Comparing and benchmarking national dementia strategies and policies. A report from Alzheimer Europe.
7. Alzheimer Scotland (2024) Commission on the Future of Long Term Care in Scotland report.
8. Healthcare Improvement Scotland (2024) Ageing and Frailty Standards.
9. Livingston, G. and others (2024) Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission.
Related website blogs:
1. The potential benefits of community support in action https://improvingcareand.education/23/02/07/community-support-in-action/
2. Approaches towards inclusive living for people in need of care https://improvingcareand.education/2023/09/19/approaches-towards-inclusive-living-for-people-in-need-of-care/
3. Music as the Carer’s Friend and Assistant https://improvingcareand.education/2023/12/11/music-as-the-carers-friend-and-assistant/
4. Communication Matters https://improvingcareand.education/2024/03/28/communication-matters/